Breast Pain - Mastalgia
Mastalgia is the Latin word for breast pain and affects more than 3/4 of women in their lifetime. The breast is a distinctive gland in the body, with a rich nerve supply and affected by fluctuating hormone levels. As a result, the breast can feel full, swollen or tender and be the site of referred pain.
Background
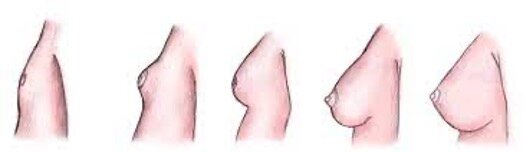
The breast is a unique structure. It grows from a tiny ‘breast-bud’ in a prepubescent girl, to a larger, fully developed gland in an adult woman, that can produce around 1 L of milk per day during lactation. It possesses a wide range of cells including nerve cells, secreting glands, ducts, the unique structure of the nipple areolar complex (NAC) as well as structural cells to provide shape.
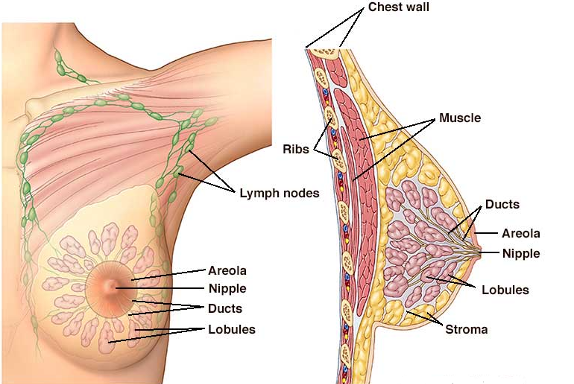
Figure 1. Stages of Breast Development
The breast is also uniquely involved in sexual excitement and arousal, with a rich nerve supply and connection to the brain and sexual organs.
Anatomy
The breast sits on the chest wall, over pectoralis major, with a tail of tissue towards the axilla (the armpit). The axilla is the intersection of several different muscles groups with overlying fibrous tissue (fascia) and therefore has a wide range of mobility. It also houses the axillary lymph nodes, which drain lymphatic fluid from the chest, arm and upper back.
Figure 2. Breast and chest wall anatomy
Hormonal influence
Normal menstrual cycle
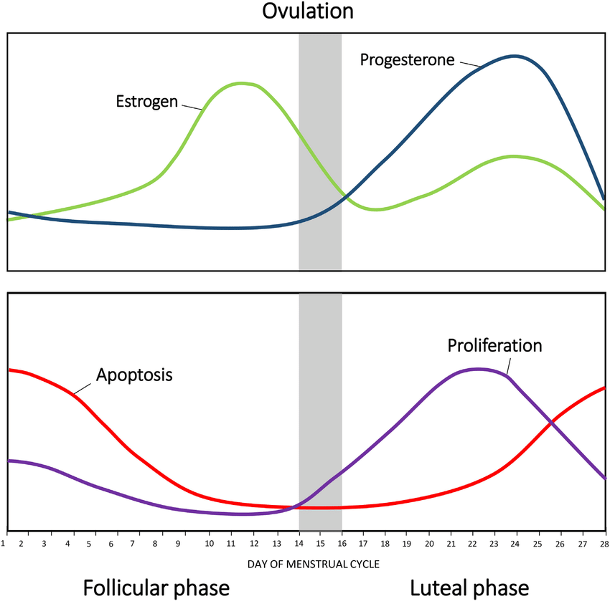
The breast responds to the cyclical change in hormone levels throughout the menstrual cycle. After ovulation, receptors receive the stimuli for growth during the luteal phase (proliferation), preparing for pregnancy. However, if no pregnancy develops, the stimulus stops and the cells of the breast start to breakdown (apoptosis).
Figure 3. Breast changes throughout the menstrual cycle
Hormonal Contraception
Women who are on the oral contraceptive pill (OCP) have consistent level of hormones being delivered to the body, therefore the breast does not undergo cyclical change. Conversely women who have a hormone secreting intra-uterine device (e.g. Mirena) have normal fluctuations in the hormone levels, as the device does not provide sufficient hormones to change the amount in the blood stream. Therefore, the breasts will undergo changes due to hormone fluctuations. Post-menopausal women produce much lower amounts of oestrogen and progesterone and therefore do not experience this cyclical variation.
Causes of breast pain
Cyclical
Most commonly, pain is due to the effects of hormonal fluctuations on breast tissue. With proliferation, there is increased blood flow and swelling in the breast. This can lead to engorgement and discomfort. As the period begins, accompanied by breast cell breakdown, tenderness will reach its maximum then start to improve.
A pain diary can help identify if pain is associated with the latter half of the menstrual cycle and menses.
As women enter perimenopause, with irregular ovulation and fluctuating hormone levels, there can be increased swelling and discomfort in the breast, because of dropping progesterone levels.
Non-cyclical
Breast pain that is not related to the menstrual cycle is called non-cyclical. This is usually caused by conditions that consistently affect the breast, not influenced by hormones. The most common of these is fibrocystic disease of the breast although pain can occur with no abnormality identified in breast tissue.
Figure 4. Fibrocystic disease of the breast
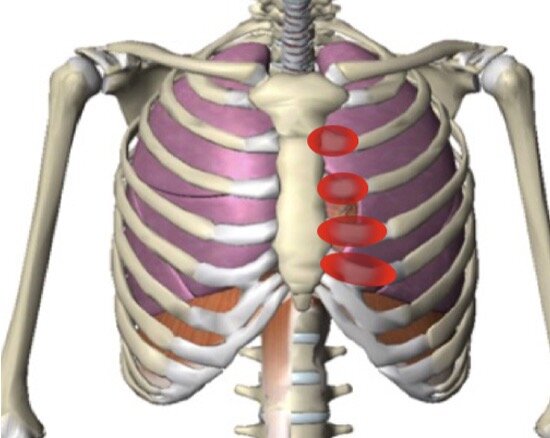
Musculoskeletal
Muscular and bony causes of chest wall pain are very common, such as inflammation of the joint between the ribs and the breastbone (costochondritis). In addition, muscular strain of the nearby muscles is not uncommon and could be due to recent unusual activity – lifting, reaching, repetitive use.
Figure 5. Costochondral joint inflammation
Investigations
It is important to undergo high-quality imaging to exclude any serious pathology. Patients over the age of 40 should have a mammogram and an ultrasound, while those under 40 should undergo an ultrasound.
Some patients may need the addition of an MRI if their breast imaging has been limited due to increased breast density (BIRADS D).
Management
If serious diagnoses have been excluded, treatment turns to a management approach, to minimise factors that can aggravate or contribute to discomfort.
Bra
A well-fitting bra is very important. Changing hormone levels and body habitus contribute to a change in breast size and composition throughout life. Changing muscle mass and posture can change the shape of the rib cage, meaning both chest circumference and cup size should be remeasured every few years plus after pregnancy, lactation or weight change.
Simple analgesia
For discomfort due to any type of mastalgia, paracetamol and/or anti-inflammatory medication can provide symptomatic relief. Some patients may need this for several days each month. Heat packs can also be useful.
Other supplements
The following have limited published evidence around their utility but are safe and can contribute to improved overall well-being.
Evening Primrose Oil – 1000mg twice a day for 2-3 months
Minimising caffeine
Minimising Alcohol
Oral Contraceptive Pill
Very occasionally, women with severe cyclical mastalgia may consider the OCP to reduce the hormonal fluctuations affecting their breasts.
Acupuncture, physiotherapy, yoga
Can all assist with pain management as well as treating musculoskeletal pain.
Mastalgia is a common condition affecting most women at some time in their life. Understanding why it is occurring can help when choosing a management plan, to ensure pain causes minimal disruption to your life.